
Real stories
Applying for NHS Continuing Healthcare – Caution, requires extreme strength of character
Mark's story highlights how it is people with dementia who fall between the cracks between health and care, and that NHS Continuing Healthcare - an option for so few people with dementia, for such a limited time – is another example of our broken system.
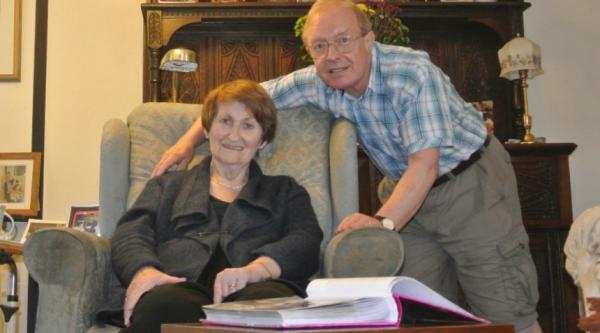
Mark Chipperfield, Alzheimer’s Society supporter, tells the story of his mum Jean and his family’s nine year battle with the support system that they thought would help them.
My mother Jean, a former nursing sister, was diagnosed with Alzheimer’s in 2008. Six months later her world disintegrated with the death of her husband of 40 years, Ben. My family’s world also started on a long and difficult path to support her to stay in her own home.
Mum’s dementia rapidly developed after Dad passed away. I had promised my father I would try to help mum stay in her own home, but I could see she needed help with, what to me was a severe health issue. So I recruited part-time carers, but then I discovered NHS Continuing Healthcare (NHSCHC).
I initially asked for my mother to be assessed. The then Primary Care Trust (PCT) assessed my mother, but I was informed that should she be awarded funding, I would lose control of arranging the care myself and the NHS would take over any plans for my mother. So she was unlikely to be able to stay in her own home.
A difficult journey
That set the tone for what has been a long, arduous, unprofessionally managed, overly bureaucratic, inhumane journey and terrible relationship with the PCT and subsequent Clinical Commissioning Group (CCG).
It has been a ‘fight’. Not what we should expect from an NHS department, which seemed only concerned about not awarding funding, and had little interest in the health and well-being of someone suffering from a degenerative, awful, unpredictable illness, that is experienced differently by all its victims, but massively impacts all of them.
My mother was turned down three times during the assessments for NHS Continuing Healthcare.
By my third attempt in 2011, I also had an on-going complaint running against the handling of the process. I presented my case, there was a bit of ‘feedback’ from the experts, and later I was sent a report showing that the local NHSCHC team had acted properly. I was amazed. It seemed like a conspiracy, a closed shop, the NHS marking the NHS and finding the NHS not guilty. I was devastated, crestfallen, but also incensed, and determined to overturn this somehow.
At the end of 2012, we were advised we were eligible for funding. The CCG provided funding, but very little other support at all. Fortunately the health agencies, GPs and nurses were wonderful, supporting what we were trying to do.
Funding removed
In 2016, the CCG ran another eligibility test and despite mum’s obvious extensive health deterioration, funding was withdrawn. We had a magnificent team and set up that helped provide my mother with some kind of positive life despite everything – and the CCG had removed themselves from any responsibility. It was shocking. I couldn’t really believe it.
My mother’s health deteriorated further and she was hospitalised with pneumonia. The doctor said she was not strong enough to recover. I made the decision to transfer her home where she passed away on New Year’s Day, surrounded by love and some of her care team.
I will see this case through but I have been appalled by the way an NHS department have failed both my mother and the taxpayer. My mother died unfunded and uncared for by the CCG, with us fearing about the future when her own funds ran out.
Mum had been in the palliative cohort with her GP, since 2015. Her conditions were clearly impacting her far more than in 2012 when funding was awarded and to my mind it was totally unacceptable to remove the security of funding later on. Not everyone will be eligible, but once provided, the process of removal should arguably be even more thorough. This was not the case for our family.
Join our campaign for quality social care
You can stand with us to ensure that people affected by dementia are heard loud and clear on their demands for social care reform. Become a campaigner to stay up to date with the latest Alzheimer’s Society news and to support future campaign actions.


Charlotte
saysCCH is based on the needs of how bad the person is, I.e are they incontinent/doubly incontinent. Can the person dress them selves with out assistance? Are they can they be inclined to be violent, ..personally I think all older people of this generation should get free care, Alzheimer's of any type is a cruel disease, I don't feel decisions are made on ethnicity, that's an unfair comment, or perhaps one made in anger? I fail to see why a drug addict is given numerous opportunities for free rehab, alcoholics given free rehab if required, but if your elderly and frail and end up with a disease that affects your entire way of living you have to pay. Obviously if the person becomes unwell and has a husband or wife this does not mean selling your house from under you. But I do feel as it can effect your life savings it's something that the government need to change, I have been round a few nursing homes and I would be heartbroken if I had to lose my money to the care that is given in some. People should be allowed to keep their money, then donate it to the cats protection society if the want to. The Government need to find somewhere else to drain money from and allow these people the help they need.
Ann
saysOmg this is so shocking to read all these stories , I was just about to start the journey of applying for chc funding, I have lost faith now. I think it’s appauling that you have to fight kicking and screaming for what should be there for all who are suffering 😡
Karen Stone
saysI have tried again recently to get CHC funding for my mum.. my mum cannot do anything for herself and has to be cared for in a care home. I lost my mum 2 years ago to this terrible disease. It is so hard for our family to slip our mum slip away like this. My dad goes every day to see her and feed her. I believe that the system should be changed and the goal posts moved and the criteria required to meet CHC requirements.
Mrs Elaine L Trimm
saysI applied for it with my dads cancer diagnosis then again when he was terminal and then again when he was given 7 days to live and i got told it depended how quietly he died meaning if he kucked off he would get it cause it would require more nurses to deal with him even after they told me he wasnt allowed to go home had to go into a nursing home they never gave it to him
Sally Best
saysMy mum had alzheimers on top of the complex condition arachnoiditus which is a very painful spine condition. She had also had a stroke. Apparently her needs were not complex enough to warrant continuing care! We were met with a determination not to fund her. I felt that the assessors main goal was to block funding. A very heartless and cruel process. We were subjected to the system a second tome with my dad who developed vascular dementia. Again a cruel determination not to fund care. For two years the cost of vare for both was almost two thousand pounds a month. We wouldn't begrudge a penny if the system wasnt so scewed to denying care that dementia sufferers shoukd be entitled to.
Yvonne Tobin-Walker
saysMy widowed Mother was diagnosed with Alzheimer's & Vascular dementia in 2012. As she had more than the baseline amount in savings she had to pay for her own care.
With help from self-funded carers & our family, she managed to stay in her own home for 4 years. She deteriorated to the point where she would need 2 carers 4 times per day, & shortly after, 24 hour care which resulted in her having to go into a care/nursing home in 2116. By 2017 her condition had worsened to the degree whereby she could no longer feed herself, take her own medication, support her own body weight, was doubly incontinent, suffered grade 4 pressure sores/ulcers, could no longer move her fingers & limbs due to contracture of the muscles, suffered frequent UTI's, didn't recognise us most of the time, couldn't speak & spent 90% of the time with her eyes closed. So we started the process of applying for CHC. She passed the first checklist, then her case got lost in the system. 6 months later it was picked up & had the MDT meeting & DST assessment. We were told she didn't qualify for CHC, only for NHS Nursing funding which was mimimal, however my Mum didn't get the amount knocked off her £3900 per month bill - the Nurses at the home got it as her nursing care was provided by nurses in the home rather than district nurses. My Mum sadly passed away 6 months later. 4 months after that (Aug 2018) we decided to appeal using a recommended specialist solicitor. We are still awaiting a result, its not the solicitors who are dragging their heels but the CCG. They've had all Mum's care records from the nursing home/GP/Hospitals/Clinics, and we've recently had to pay extra to acess more records. Basically the CCG make it as difficult as possible for people to get funding, put hurdles up every step of the way in the hope that they get fed up & give up. All the departments ie: social workers/nurses/CCG/assessors are all working for the NHS/Authority so the whole thing is set up to fail. We are appealing as a matter of principal as we feel our Mum was failed by the NHS/Government after she & my Dad worked hard all their life to get what they had & for their family. Good luck to all of you on this heartbreaking distressing journey.
Fiona
saysMy mother became totally dependent for all of her care following the rapid onset of vascular dementia. She also had hypertension, type 2 NIDDM and AF, she had been on warfarin for a number of years following a TIA.
We could have applied for CHC whilst she was still in hospital but that would have restricted which nursing homes she would have taken her. We elected to choose a nursing home that we felt would provide the best care for her as an interim solution and when the disease progressed we would apply for CHC.
We applied in November 2018 and were ‘forgotten’ about despite asking a few times, when we finally had the assessment, 6 months later the criteria was so tough it was laughable, because she was able to say no to having a blood sugar test (finger prick) they tried to say that she was able to make decisions about her care, despite the fact that she was unable to meet any of the Activities of Daily Living.
Basically if you sat her down with food, drink and her medications next to her and left her for 24 hours, she wouldn’t have moved, wouldn’t have eaten, drunk or taken her meds, she doesn’t know that she needs the toilet and isn’t weight bearing but she still had to be fully assessed and scored.
Tony Shields
saysMy wife self-referred herself to her GP because of her failing memory. The GP arranged for an NHS assessment by a psychologist and psychiatrist. Their initial assessment was 'mild cognitive impairment'. She was referred to the local hospital for six-monthly MMSE assessments; over the next four years her MMSE performance dropped but not to the extent that she was seriously affected by her memory loss. I was her sole carer over the initial period of approx 5 years. We moved geographically from Buckinghamshire to Essex in order to be closer to our son and his family.
At that time I began to seek third party support for my wife and myself. As the result of a telephone by Social Services I was told I was obviously doing a great job and SS felt there was no requirement of support. It was emphasised the actually I needed to look after myself so I could continue to support my wife. As part of her six-monthly MMSE checks and visits by support services arranged by our local GP, I was always told what a good job I was doing and I needed to look sfter myself. When I commented "I am not your patient, my wife is. What help can you offer her?" At which point they disappeared over the hills. I eventually bought my own support services: a weekly cleaner, daily carer, chiropodist.
Other articles above have absolutely shocked (and annoyed) me. In the seven years my wife suffered from dementia I had NEVER HEARD of CHC. NEVER!
Eventually my wife had to be looked after by a Care Home. She eventually had to be taken into hospital. I was asked to join the care consultation. At that point they offered a fully financed and supported End of Life Palliative Care Programme. It took the sister at the hospital a full day to argue the case with the CCG - she achieved it, it would seem against all the NHS's arguments. My wife lived for a further eight weeks under the brilliant care of the Care Home supported by the hospital.
Having read all the report and comment the disgrace is that there is no common ground in the provision of support for dementia. Also it is a disgrace that it is seen as a "social problem" and not as an illness.
I could add more but that might get me even more angry about the lack of effective support.
Orphan Annie
saysI sympathise with you all. It is only the people who have tried to navigate this very flawed system, at the most stressful time if their life, who really understand.
As my Mother’s dementia became more noticeable (and problematic) to outsiders, I was told that she would ‘have to ‘ go into a care home. At the time I found it really heart breaking that she would be leaving her lovely flat in sheltered accommodation and I would be visiting her in a care home - something that I had said I would never let happen.
As it turned out Mum settled well and surprisingly liked it there. I visited daily and brought her to my home or took her out for the afternoon frequently.
Everything went pear shaped when my Mother fell poorly and the GP was too busy to visit! The home were told to call an ambulance if they were concerned. They did and everything plummeted from there.....
My Mother was emotionally and physically abused on the ward, which was reported by a whistle blower. This resulted in a deterioration of her dementia and my Mother was placed in an EMI home. I asked for a CHC assessment prior to discharge only to be told it is for end of life care.
My Mother went into the new home without support, having had 1:1 care following the abuse and extremely heightened anxiety.
She had 15 falls in 2 weeks at the home and broke her neck,; they were short staffed. She ended up on an orthopaedic ward for three months with the non healing neck fracture and refusal to wear the neck brace. I requested CHC meeting again and got funding (following two heated meeting) for her to have 1:1 nighttime care at night in a new EMI to manage the night terrors and to prevent her from falling again and causing more damage to her neck, or worse. This was granted for4 weeks initially.
At the end of the four week period there was another meeting to say the funding was being withdrawn! I couldn’t risk my Mother being left without support and the new care home said they couldn’t manage her without the support so she would have to leave. After another heated battle I managed to eventually convince everyone that I could look after my Mother at home. I was delighted to bring her to live with me and regretted not fighting before ... I didn’t know I could.
I took my Mother to a specialist spinal centre for a follow up appointment after breaking her neck and the consultant told me that I should have been in receipt of CHC!!!! The appointment was at a hospital over the border in England and we are in Wales - I was told it’s a bit different there. As I was paying nearly £700 a week (my money, another family member’s contribution and my Mother’s small pension) to pay for someone to sit with her all night, as she never slept following the abuse and associated fear, I decided so should apply again as it was financially crippling- but worth it!
Two more heated meetings at my home, months of battles between heath and social services then support was granted during my Mother’s last week of life when she was in hospital.
I had my Mother at home for a year where she was happy and properly cared for. If only I’d have realised earlier that I could challenge the system. Whilst her needs were complex she presented far better at home than in residential care.
At first, after she passed away, I was too heart broken to do anything, but now I have put in a complaint about the CHC process to the local health board. If nothing else it will hopefully ruffle some feathers and make them think twice about how they apply this framework.
I would be more than willing to help anyone else going through something similar.
Learning to support someone with this terrible condition is stressful enough without having to deal with the inadequacies of the CHC process.
Paul Wood
saysCan you help me I have requested an Independent Review Panel, but it will be delayed due to the Corona Virus outbreak.(7 years up to this date)
Anonymous
saysHi Paul
We recommend speaking with one of our dementia advisers on 0333 150 3456. They can listen to your situation, provide advice and support. Our advisers are available seven days a week. You can find opening hours for our Dementia Connect support line here: https://www.alzheimers.org.uk/get-support/dementia-connect-support-line
We hope this helps, Paul.
-
Alzheimer's Society blog team
Shelly
saysAs a family we were declined CHC 2 times and the assessment process causes distress to the person and is completely flawed. In our case the CHC assessor informed us she would be accessing doctors records for a record of all health appts etc as well as prescribed medication. I knew this would be a blot on the health assessment and would affect the points scoring system because in our case as a family we decided to withdraw all tablets and appts because frankly the medication reached a point where it stopped working, just as the psychiatrist had mentioned when he first prescribed it. As for health appts we felt they were no longer needed because there is nothing anyone can do or give you to stop the dementia. I asked the psychiatrist would there come a point when the medication would plateau and he said yes and I then asked how would we know to which he replied you may see increases in the earlier signs you saw. So we decided to bear this in mind and several years after being given medication and after having several psychiatric appointments cancelled due to a shortage of doctors, we took it upon ourselves to do a slow withdrawal.
CHC had nothing to record in terms of medication and appts and this greatly reduced our scores for CHC.
However we still had to deal with someone who couldn’t do anything for themselves from drinking to feeding and washing and dressing, someone who was doubly Incontinent who smeared faeces and was at risk of touching her mouth and food and spreading infection through other channels, had we not been with her 24/7 and observed her so throughly. No nursing home in the country could have provided the intensity of observations and care as we did. It was hard work with a consistent rota of four family members but absolutely brilliant for the person with dementia because they were in their own house surrounded by love and care.
Professionals see dementia as behavioural and not as a health need but the disease is no different to cancer in some ways in that it results in death but unlike cancer you can’t get an approximate prognosis . It’s a slow death that strips you of your dignity and humanity. The CHC document is flawed from beginning to end .
Ann morton
saysI feel upset when I have been reading these comment my husband has alzimers and vascular dementure also heart failure I haven’t asked yet for help put Iam sure I will need it
Geoff Lindsay
saysCHC can pay for carers to keep you in your own home. I worked as a Registered Social Worker specialising in older persons mental health. There is institutional discrimination at work preventing many people from getting NHS funding. What works in keeping people living safely and well at home, is maximum 2 carers per week, with minimum 1 hour visits. Pay more for qualified home carers, about £15ph gross. When care homes can charge hundreds of £s pw, it is worth it.
Pat Savage
saysThe CCG's and Local Authorities pass the funding issues from one to t'other,and have hand-to-mouth funds. It is wholly and ethically wrong that many patients who are legally entitled to CHC are passed over because they don't have belligerent relatives to fight their case. My mother was assessed as eligible for CHC but it was six months before her Independent nursing home( she has advanced AD/vascular and Diabetes 1) received any monies from the CCG. We were then told she had to "top-up" the award herself as it was her "lifestyle choice" to remain in that particular home. Any NHS full-funding care is FREE at point of need. That includes care,food,accommodation...the LOT! It is illegal to top-ups CHC,once agreed. Keep pushing,send documents registered post and note all telephone calls. He who shouts loudest wins. Appalling yes,but stand firm!
Hazel bradley
saysMy mother was turned down, despite the fact I do EVERYTHING for her. If I didn’t she would die in a week! I’ve even given up work ( as a nurse) to care for her.... looking after a family member with dementia is a daily battle, one shouldn’t have to fight the authorities for help as well. The system is a disgrace.
HelSan
saysWe got my dad's CC two years after his death backdated to the day he was admitted to his care home. He was initially assessed and found to qualify. The person who did the assessment left the authority soon after and the assessment disappeared. Further assessments showed he didn't qualify. I sat in for one of them. I said dad didn't just do that and you marked Yes. She said, I know he can do it really though! Fight to get it and remind them they have to pay interest, We got it all eventually. My dad would be pleased nw.
Pagination